Stress is often linked to various health problems, including ulcers. While stress alone may not directly cause ulcers, it can exacerbate symptoms and complicate the healing process. This article explores the connection between stress and ulcers, types of ulcers, symptoms, and practical tips for prevention and management.
Many people wonder, can stress cause ulcers or can stress cause mouth ulcers, especially during prolonged periods of emotional or physical strain.
What is an Ulcer?
An ulcer is a sore that develops on the inner lining of the stomach, upper small intestine (duodenum), or esophagus. The most common type is a peptic ulcer, which includes gastric ulcers (in the stomach) and duodenal ulcers (in the small intestine).
Contrary to popular belief, stress and spicy foods are not the direct causes of ulcers. Instead, the main culprits are:
- Helicobacter pylori (H. pylori) bacterial infections.
- Long-term use of non-steroidal anti-inflammatory drugs (NSAIDs).
However, chronic stress can weaken the immune system and worsen ulcer symptoms by increasing stomach acid production and altering gut health. This explains why patients often ask can stress cause stomach ulcers when symptoms worsen during stressful times.
Early diagnosis and proper treatment are essential to avoid complications like bleeding or perforation.
Types of Ulcers
- Peptic Ulcers:
- Found in the stomach and upper small intestine.
- Symptoms include abdominal pain, bloating, and nausea.
- Ongoing stress may aggravate pain and delay healing, leading many to question can stress cause stomach ulcers in daily life.
- Stress Ulcers:
- Caused by physical or physiological stress, such as severe injury, infection, or organ failure.
- Common in patients in intensive care units (ICUs).
- Mouth Ulcers:
- Painful sores on the lips, tongue, or cheeks, often linked to stress and weakened immunity.
This is why doctors are frequently asked can stress cause mouth ulcers, especially during emotional exhaustion or lack of sleep.
Can Stress Cause Mouth Ulcers?
Yes, can stress cause mouth ulcers is a common and valid question, and the answer is yes. Stress is a well-known trigger for mouth ulcers, especially recurrent aphthous ulcers. When a person is under emotional or mental stress, the body releases stress hormones that can weaken the immune system. This makes the lining of the mouth more sensitive and slower to heal. During stressful periods such as work pressure, exams, lack of sleep, or emotional strain, people often notice ulcers appearing more frequently or lasting longer. Medical research and clinical experience both show that stress does not infect the mouth directly, but it lowers the body’s natural defence, creating the right conditions for ulcers to develop. This is why many doctors confirm that can stress cause mouth ulcers is not a myth, but a proven health link.
How stress contributes to mouth ulcers
- Stress weakens the immune response, making the mouth lining more prone to injury and inflammation.
- Hormonal changes during stress can delay healing of small mouth injuries.
- People under stress may bite their cheeks, clench their jaw, or grind teeth, which damages oral tissues.
- Stress can reduce saliva flow, leading to dryness and irritation inside the mouth.
- Poor sleep and irregular meals during stress also increase the risk of ulcers.
- Studies show higher ulcer occurrence during stressful life events, supporting that can stress cause mouth ulcers repeatedly.
Stress alone may not be the only cause, but it plays a strong role. Managing stress, maintaining oral hygiene, and eating balanced meals can reduce flare-ups. If ulcers keep returning, medical advice is important to rule out other causes and prevent complications.
Stress and the Gut: The Gut-Brain Axis
The gut-brain axis is a two-way communication system between the brain and the gut. Stress can disrupt this axis, leading to:
- Increased gut permeability (“leaky gut”).
- Altered gut motility.
- Changes in gut microbiota.
Stress hormones like cortisol and adrenaline further impair digestion and increase stomach acid, which can contribute to conditions like gastric ulcers.
Persistent throat irritation during high stress has also raised concerns about can stress cause throat ulcers in some individuals.
Managing stress is crucial for maintaining both gut and mental health.
Can Stress Cause Ulcers?
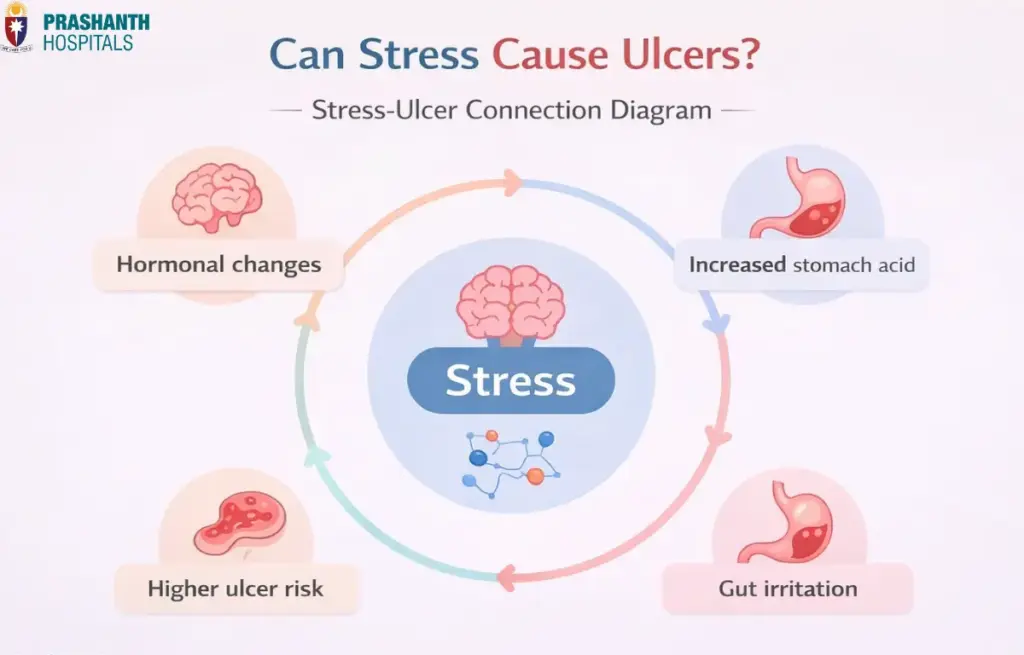
While stress is not the primary cause of ulcers, it can trigger or worsen symptoms in the following ways:
- Stress hormones like cortisol increase stomach acid production, irritating the stomach lining.
- Chronic stress weakens the immune system, reducing the body’s ability to fight infections like H. pylori.
- Stress can lead to behaviors like smoking, alcohol consumption, and unhealthy eating, all of which increase ulcer risk.
These factors reinforce why people continue to ask can stress cause ulcers when symptoms flare up during stressful periods.
Symptoms of Stress-Related Ulcers
Stress-related ulcers share symptoms with peptic ulcers, including:
- Abdominal pain or burning.
- Nausea or vomiting.
- Bloating and indigestion.
- Loss of appetite or weight loss.
- Black, tarry stools (indicating bleeding).
In severe cases, ulcers caused by stress may lead to complications such as bleeding or perforation.
Long-term stress can also worsen oral health, which explains concerns about can stress cause mouth ulcers in recurring cases.
Lifestyle Changes to Prevent or Manage Ulcers
Implementing lifestyle changes can help prevent or manage ulcers and reduce stress-related health issues:
- Dietary Changes
- Include high-fiber foods, probiotics, and low-acid options.
- Avoid junk foods and large meals close to bedtime.
- Stress Management
- Practice mindfulness, meditation, and yoga.
- Engage in regular physical activity to reduce stress and improve digestion.
- Avoid Harmful Substances
- Quit smoking, as it hinders healing and increases ulcer risk.
- Limit alcohol intake to avoid stomach irritation.
- Medical Care
- Minimize NSAID usage or switch to safer alternatives.
- Follow prescribed medications for ulcer treatment.
- Healthy Habits
- Drink plenty of water to aid digestion.
- Ensure sufficient sleep to maintain overall health.
Stress Ulcers: Understanding Their Causes
The term stress ulcers refers to ulcers that develop due to severe physical stress. Common triggers include:
- Critical illness or injury.
- Prolonged ICU stays.
- Serious infections or surgeries.
These ulcers are often seen in hospitalized patients and require careful monitoring and treatment.
How to Manage Stress for Better Digestive Health
Since stress plays a significant role in aggravating gastric ulcers, incorporating stress-reduction techniques into your routine is essential:
- Practice deep breathing exercises or progressive muscle relaxation.
- Maintain a balanced work-life schedule to reduce mental strain.
- Build a support system of family and friends for emotional resilience.
Chronic tension in the neck and throat area has also led experts to explore can stress cause throat ulcers in prolonged stress conditions.
Conclusion
While stress alone does not directly cause ulcers, it can act as a trigger and worsen existing conditions. Understanding the connection between stress and ulcers is vital for prevention and management. By adopting healthy lifestyle habits, managing stress, and seeking medical care when necessary, you can protect your digestive health and overall well-being.