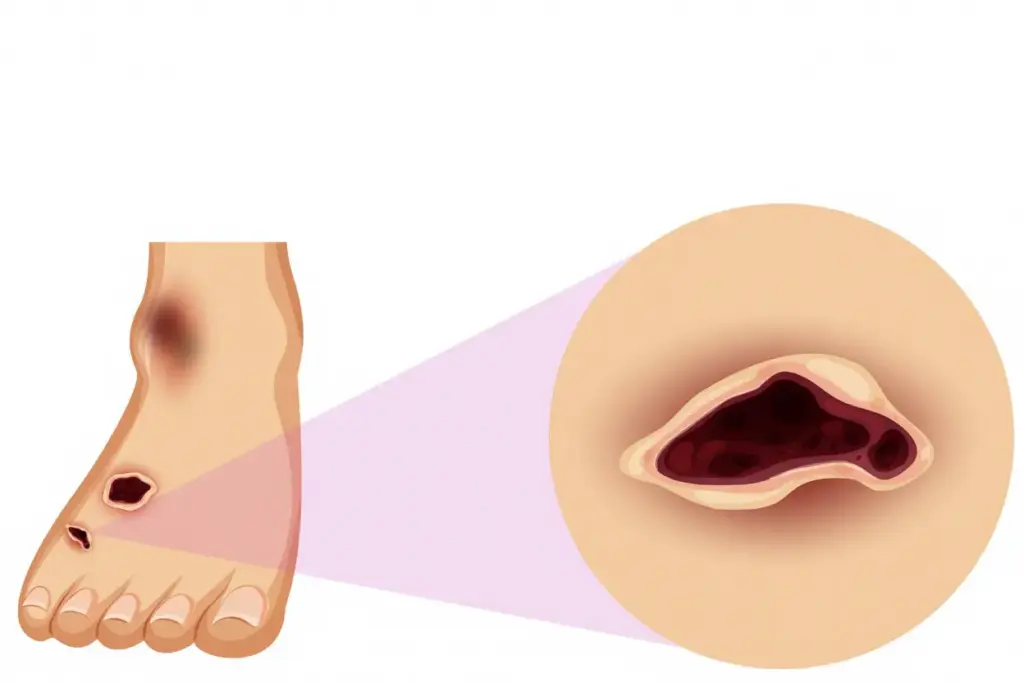
For millions of people living with diabetes, foot health is an often-overlooked yet critical aspect of managing the disease. A common and serious complication is the development of foot ulcers — open sores or wounds that are slow to heal and prone to infection. But why do diabetics get foot ulcers?
Understanding the diabetic foot ulcer causes, knowing the risks, and learning effective prevention strategies can make all the difference in avoiding this debilitating condition. This article explores why foot ulcers occur in diabetes, who is at risk, and how to keep your feet healthy.
Why Do Diabetics Get Foot Ulcers?
Foot ulcers affect about 15% of people with diabetes at some point in their lives. They occur due to a combination of factors that stem from high blood sugar levels over time. Here’s a closer look at the main reasons:
Poor Circulation (Peripheral Artery Disease)
High blood sugar can damage blood vessels and reduce blood flow, particularly to the extremities. This condition, called peripheral artery disease (PAD), means that less oxygen and nutrients reach the feet, making it harder for wounds to heal. Even minor cuts or blisters can quickly develop into ulcers when circulation is compromised.
Nerve Damage (Neuropathy)
One of the most common complications of diabetes is peripheral neuropathy, or nerve damage, which often affects the feet. Neuropathy causes reduced sensation, so you may not feel pain, heat, or pressure. Without this natural warning system, small injuries can go unnoticed and untreated, turning into ulcers before you’re even aware there’s a problem.
High Blood Sugar and Slow Healing
Uncontrolled blood sugar impairs the body’s natural healing ability and weakens the immune system. This creates the perfect environment for infections to develop and for minor wounds to progress into serious ulcers.
Foot Deformities and Pressure Points
Many people with diabetes develop changes in the shape of their feet, such as bunions, hammertoes, or collapsed arches. These deformities can create areas of high pressure inside shoes, leading to blisters and sores that are slow to heal — another key reason why diabetics get foot ulcers.
Risk Factors for Diabetic Foot Ulcers
While anyone with diabetes can develop foot ulcers, certain factors increase your risk:
- Long-standing diabetes (especially over 10 years)
- Poor blood sugar control
- History of previous foot ulcers or amputations
- Smoking (which further damages circulation)
- Obesity
- Wearing ill-fitting shoes
- Vision problems that make it harder to check your feet
Understanding these risk factors for diabetic foot ulcers is essential so you can take steps to reduce your chances of developing them.
Why Foot Ulcers Are Dangerous
Foot ulcers are not just painful — they can lead to serious complications if left untreated. Infections from ulcers can spread to the bones (osteomyelitis), and in severe cases, amputation may become necessary to prevent life-threatening infections. That’s why prevention and early treatment are crucial.
Preventing Foot Ulcers in Diabetes
The good news is that most foot ulcers are preventable with proper care and awareness. Here are some practical diabetic foot care tips to protect your feet:
Inspect Your Feet Daily
Check your feet every day for cuts, blisters, redness, swelling, or discharge. Don’t forget to look between your toes and use a mirror for the bottoms of your feet if needed. Early detection can prevent minor injuries from becoming ulcers.
Wear Proper Footwear
Choose shoes that fit well, with plenty of room in the toe box and no tight spots. Avoid walking barefoot, even at home, to prevent injuries. Consider custom orthotics if you have foot deformities or pressure points.
Keep Feet Clean and Dry
Wash your feet daily with warm (not hot) water and mild soap. Dry them thoroughly, especially between the toes, to prevent fungal infections.
Manage Blood Sugar
The better you control your blood sugar, the lower your risk of developing ulcers and other complications of diabetes. Work with your healthcare team to maintain your target levels through diet, exercise, and medication if needed.
Stop Smoking
Smoking narrows blood vessels and impairs circulation, increasing your risk of ulcers. Quitting smoking is one of the best things you can do for your feet — and your overall health.
Schedule Regular Checkups
Have a podiatrist or your primary care provider examine your feet at least once a year — more often if you have neuropathy or a history of ulcers. They can spot problems you may miss and recommend preventative treatments.
When to See a Doctor
Even with the best care, you might still develop a foot ulcer. Seek medical attention right away if you notice:
- A wound that isn’t healing or getting worse
- Redness, warmth, or swelling around a sore
- Drainage or foul odor from a wound
- Black or blue tissue on your toes or feet
- Fever or chills alongside a foot wound
Prompt treatment can prevent infections from spreading and reduce the risk of serious complications.
Final Thoughts
So, why do diabetics get foot ulcers? The answer lies in how diabetes affects the nerves, blood flow, and healing process — creating a perfect storm for minor injuries to turn into serious wounds.
But with the right knowledge, vigilance, and care, you can greatly reduce your risk. By managing your blood sugar, inspecting your feet daily, wearing proper shoes, and seeking care when needed, you can avoid this common and dangerous complication.
Healthy feet are the foundation of an active, independent life — take the steps today to protect them.